Colorado has tested nearly 450,000 people for COVID-19. Right now, about 5% of daily tests come back positive. When you get tested for COVID-19, how does the test actually work? There are a few kinds of tests, with several differences between them.
When you pull up to a clinic to get tested for COVID-19, in most cases they will stick a cotton swab with an extra-long handle in your nose, twist it around, put it in a tube and notify you a few days later of the results. This is how they diagnose if the virus that causes COVID-19 is currently living in your body.
In contrast, the antibody test or serology test uses a blood sample. This test tells you if you've had the virus. It cannot determine if the virus is presently replicating in your body.
The Diagnostic Test
The diagnostic swab test looks for the genetic code of the virus. DNA makes up the genetic code in humans and most living organisms. Viruses are unique. Their genetic code can be made of DNA, like the influenza virus, or RNA, like the coronavirus. All DNA is converted into RNA to function in the cell. Humans have RNA too, we just don't store our genetic code in it.
The coronavirus only has RNA. It doesn't need to convert DNA to RNA, which means it skips a step and can replicate more quickly. When we look for the coronavirus, we look for its RNA.
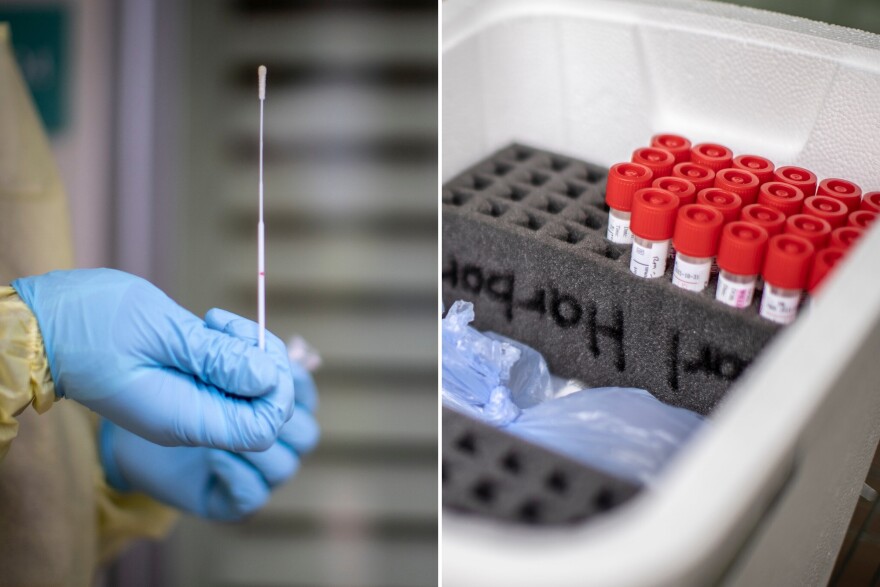
Unlike DNA, RNA breaks down quickly. The sample from our nasal cavity is put in a liquid that preserves the RNA, called "viral transport media," and must be kept cold. The test checks for human RNA to make sure the sample is in good condition.
"Most of the tests are also able to detect human RNA and they use that as a control, as an internal control to the test, to demonstrate that it was a good sample, that it contains human material," said Dr. Emily Travanty, scientific director at the Colorado Department of Public Health and Environment.
When the sample arrives at the lab, technicians extract all of the RNA. Human, viral, bacterial — the RNA from every living thing in your nasal cavity will be present — and they must distinguish SARS-CoV-2 (the novel coronavirus that causes COVID-19) from the rest.

To understand how this is done, imagine an enormous fruit salad, with thousands of pieces of fruit, but only four kinds: apple, tangerine, grapefruit and cherry. Instead of being in a bowl, the fruit is lined up, single file. The order of these fruits will make a code: apple, apple, cherry, apple, tangerine, etc. The coronavirus code is 26,400 "fruits" long. That code is the genetic sequence, and the order is different in every organism.
We know the genetic code of SARS-CoV-2. Researchers use short matching codes — series of about 15-20 "fruits" — to find specific viral sequences. They use tiny molecular machines, called enzymes, to first convert the RNA into DNA to stabilize the RNA, and then make lots of copies of these sequences. This process is called amplification. If the coronavirus RNA sequence is there, they can tell.
Note: Neither RNA or DNA is made of fruit, of course. They're made of nucleic acids — but the sequence is specific.
Accuracy
There are two types of diagnostic tests: a PCR test and a rapid test (also known as a LAMP test). These tests are not equal.
The PCR test is more accurate than the rapid test. As the name implies, rapid tests are fast returning results within hours, but if there's very little viral RNA, it may not be amplified — resulting in a false negative.
Dr. Travanty said that the rapid test "can give you a fast result on a positive; negative tests on that though are still refluxed to the PCR test, the traditional assay."
95% of daily tests in Colorado come back negative. Unless a patient is experiencing symptoms and had a known exposure, performing a rapid test doesn't make sense.
The PCR test is accurate and specific, provided the sample is good and managed to catch traces of the virus. A single sample run looks for three different parts of the viral genome, to make sure they don't mistake SARS-CoV-2 for a different coronavirus, like the common cold.
Both the PCR and rapid tests are vulnerable to sample-handling issues. Regardless of the type of test, if your sample isn't kept cold, the RNA will fall apart — like the lined-up fruit rolling around and getting mixed up. Human and viral RNA will both fall apart if the sample is not kept cold, so if you can amplify human RNA from the sample, the sample is good.
Travanty said tests at CDPHE include "the control that says 'Yes, I detect human RNA in the sample.' If you get a negative result for the virus, that you know there was good sample and that the RNA was in good quality when it got its way back to the lab."
Positive controls are a crucial element of a good test. Otherwise, the results are inconclusive.
The other issue could be that the swab didn't grab the coronavirus in your nasal cavity. If you were tested and the result came back negative, it's a good idea to get tested again if symptoms persist.





